Did you know that more than 30% of Americans are currently diagnosed with fatty liver disease? This alarming statistic highlights the importance of understanding this condition and taking proactive steps to manage it before things get out of hand.
This article is a supplement to two episodes of Dr. Gandolfo’s podcast The Real GI Doc Show:
“The Natural Way to Treat Fatty Liver Disease at Home” Listen to the full episode here.
“The Psychology Behind Healthy Habits: Expert Tips for Real Change with Noreen Vail, PhD” Listen to the full episode here.
What is Fatty Liver Disease?
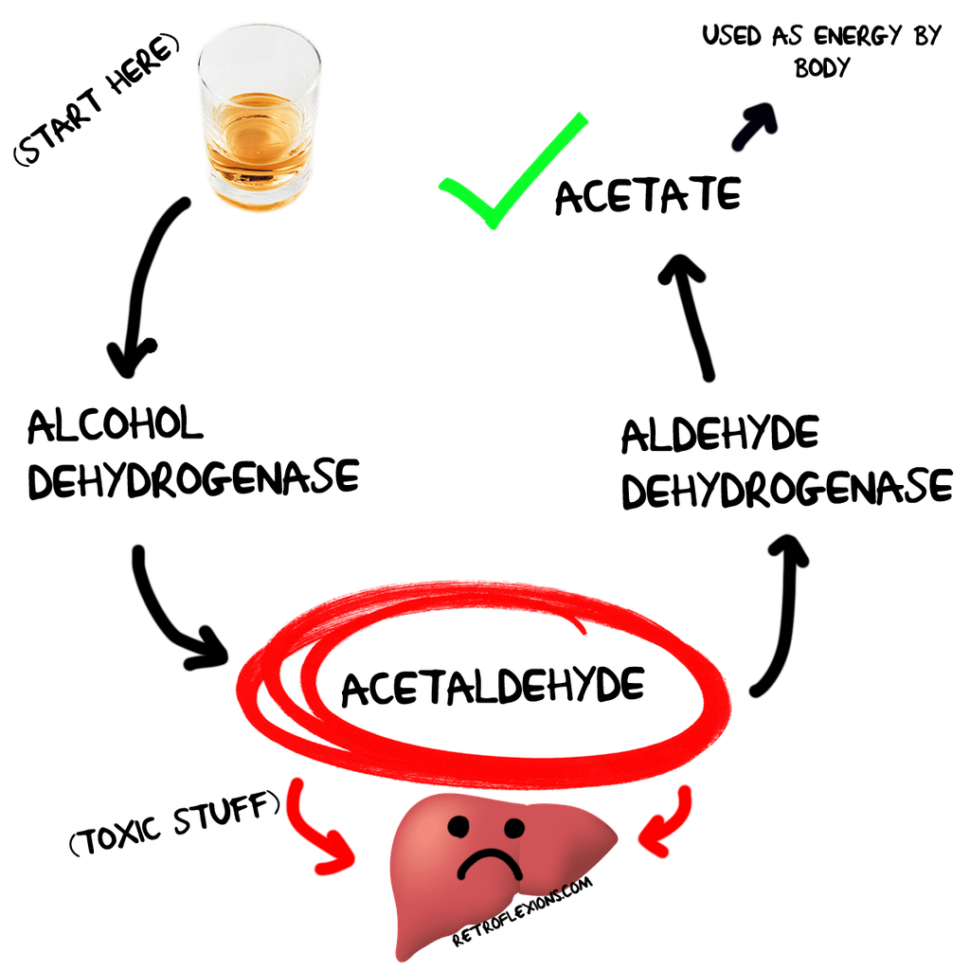
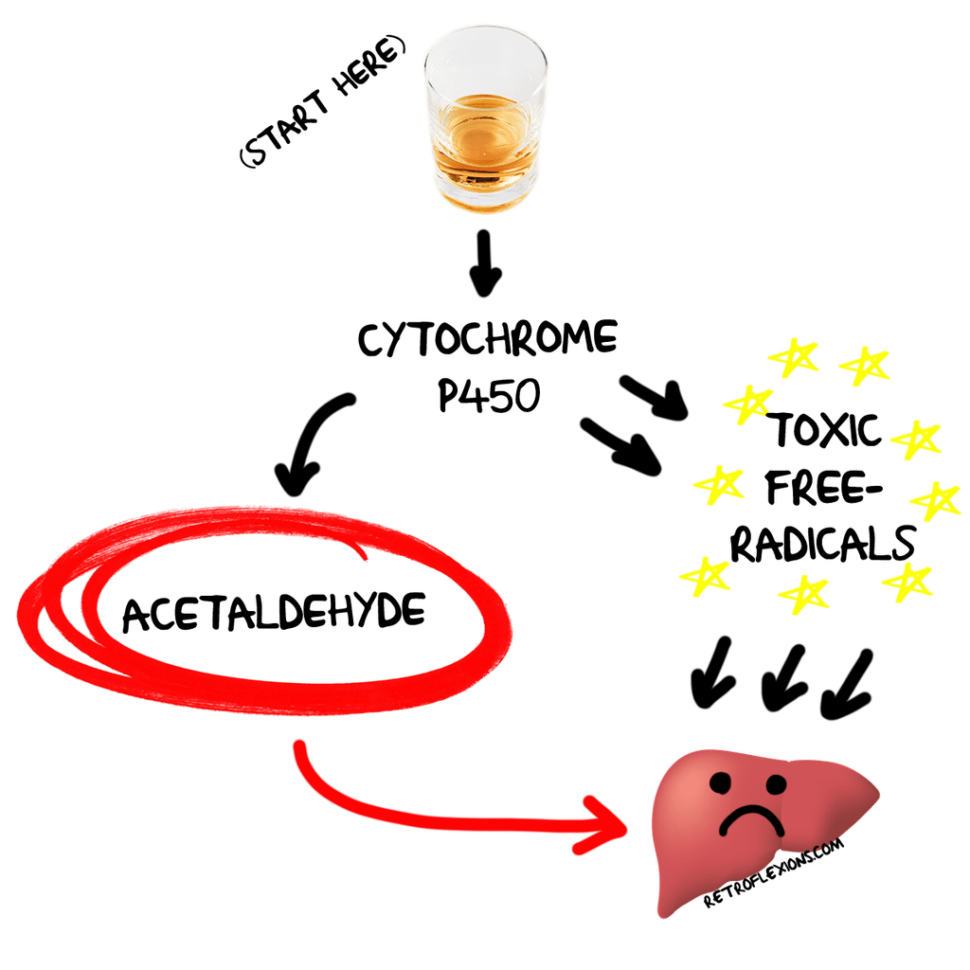
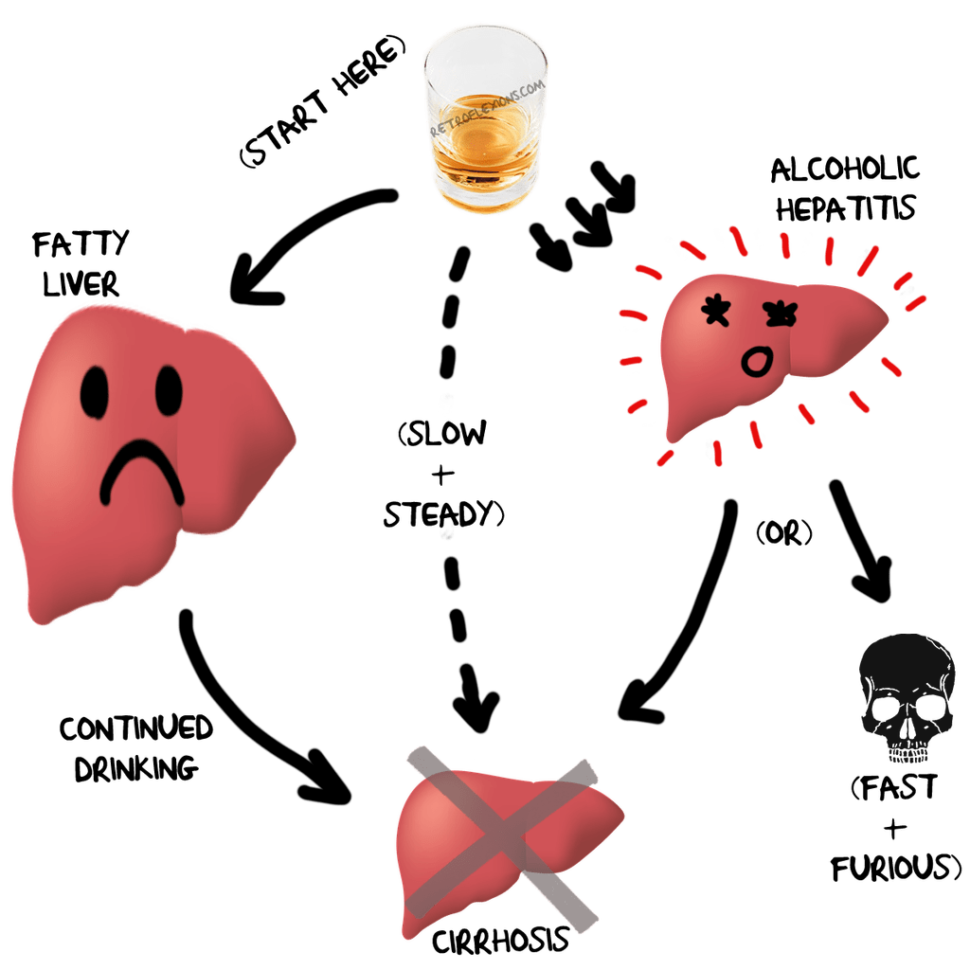
Fatty liver disease, recently renamed as Metabolic Dysfunction Associated Steatotic Liver Disease (MASLD), is a condition where more than 5% of liver cells contain fat. This can lead to inflammation, fibrosis (liver scarring), and in severe cases, cirrhosis. The condition is closely linked to metabolic issues such as obesity, type 2 diabetes, and hypertension. Understanding these connections is crucial for effective management and treatment.
Jim’s Case: A Common Scenario
In a recent podcast episode, Dr. Gandolfo introduces us to a hypothetical patient, Jim, a 48-year-old man with prediabetes and mild hypertension. Jim’s routine blood work reveals mildly elevated liver enzymes, leading to further tests that confirm he has fatty liver disease. Jim’s history is not unique, and it serves as a reminder that many people may be living with this condition without even knowing it.
The Importance of Early Intervention
By the time fatty liver disease is diagnosed, the underlying metabolic issues have often been present for years. Early intervention is crucial. Dr. Gandolfo emphasizes that the best time to make lifestyle changes was five or ten years ago, but the second-best time is right now. This proactive approach can prevent the progression to more severe liver conditions. Early detection and lifestyle modifications can make a significant difference in the prognosis of the disease.
Natural and Effective Treatments
Dr. Gandolfo outlines two primary, cost-effective treatments for managing fatty liver disease:
weight loss and exercise.
Weight Loss: A modest weight loss of 3-5% can start the healing process in the liver. For more significant improvements, especially in cases of inflammation and fibrosis, a weight loss of 10% or more is recommended. Sustainable dietary changes are key. Dr. Gandolfo suggests finding a diet that fits your lifestyle and preferences, with the Mediterranean diet being
particularly beneficial. This diet is rich in fruits, vegetables, whole grains, and healthy fats, which can help reduce liver fat and improve overall health.
Exercise: Regular exercise, independent of weight loss, improves cardiovascular health and insulin sensitivity. Dr. Gandolfo recommends moderate exercise, such as walking, swimming, or weightlifting, for at least 150 minutes per week. Building muscle mass is also crucial, as it helps to combat insulin resistance. Incorporating physical activity into your daily routine can be a game-changer for liver health and overall well-being.
The Role of Coffee
Interestingly, Dr. Gandolfo highlights the benefits of coffee for liver health. Up to three cups of black coffee a day can reduce liver inflammation due to its antioxidant properties. However, he advises avoiding high-calorie coffee drinks that can negate these benefits. The antioxidants in coffee can help protect the liver from damage and reduce the risk of liver disease progression!

The Psychology of Creating a Healthy Lifestyle
Dr. Gandolfo acknowledges the challenge many patients face in creating and maintaining these lifestyle changes. To help make these healthy changes easier, on episode 11 of The Real GI Doc Show he interviews a special guest, Dr. Noreen Vail, a licensed psychologist with a PhD in clinical psychology. Together, they delve into the psychological aspects of making lifestyle changes, particularly focusing on fatty liver disease.
Dr. Vail introduces the transtheoretical model, a well-researched framework that outlines five stages of behavioral change: pre-contemplation, contemplation, preparation, action, and maintenance. She emphasizes the importance of assessing where a patient is on this spectrum to tailor advice effectively. For instance, a patient in the pre-contemplation stage may not be ready to hear detailed diet plans, whereas someone in the preparation stage might benefit from specific actionable steps.
One of the key takeaways from the episode is the significance of setting realistic goals and keeping a journal. Dr. Vail suggests that writing things down can help patients become more mindful of their behaviors and track their progress. This data can be invaluable during follow-up appointments, providing a clear picture of what’s working and what needs adjustment.
Dr. Gandolfo and Dr. Vail also discuss the common excuses patients use to avoid making lifestyle changes, such as lack of time, holidays, or injuries. They stress the importance of consistency over perfection. Missing a day of exercise or indulging in an unhealthy meal occasionally doesn’t derail progress; it’s the long-term habits that count!
Another crucial aspect covered is the role of family support. Dr. Vail advises against nagging and instead recommends a supportive approach. Encouraging loved ones to join in on healthy activities can create a positive environment that fosters change.
Finally, the episode touches on the limitations of time during medical consultations and the importance of a multi-specialty approach. Dr. Gandolfo acknowledges the challenges posed by insurance and the need for accessible pathways to dietitians, psychologists, and other specialists.
This episode is a must-listen for anyone struggling to make lifestyle changes for fatty liver disease or any other health condition. Dr. Gandolfo and Dr. Vail provide practical advice and insights that can help you overcome psychological barriers and set yourself on a path to better health.
Take Action Today
The episodes both conclude with a powerful message: Start today. Whether it’s a 15-minute walk or a small dietary change, taking immediate action is essential for long-term health. Small, consistent efforts can lead to significant improvements over time!
For more in depth information, listen and subscribe to the show here.
Medication for Fatty Liver Disease
If you have been diagnosed with fatty liver disease, there is now an FDA-approved medication called Rezdiffra available for some patients with liver fibrosis. To see if you qualify for treatment, a measurement of your liver health is taken with a FibroScan test. This simple ultrasound test is done in the office and can determine if have significant fatty liver disease, and will also measure the fibrosis level.
To make an appointment for an assessment, send us a message here or call the office during regular business hours.