In the US, colorectal cancer is currently the second leading cause of cancer deaths in men and women combined. Virtually all health professionals agree that screening average-risk people starting at age 45 for colorectal cancer is the best way to prevent this disease. There are a few highly effective tools available for colorectal cancer screening: This article will focus on the two most popular tests, colonoscopy and the Cologuard test.
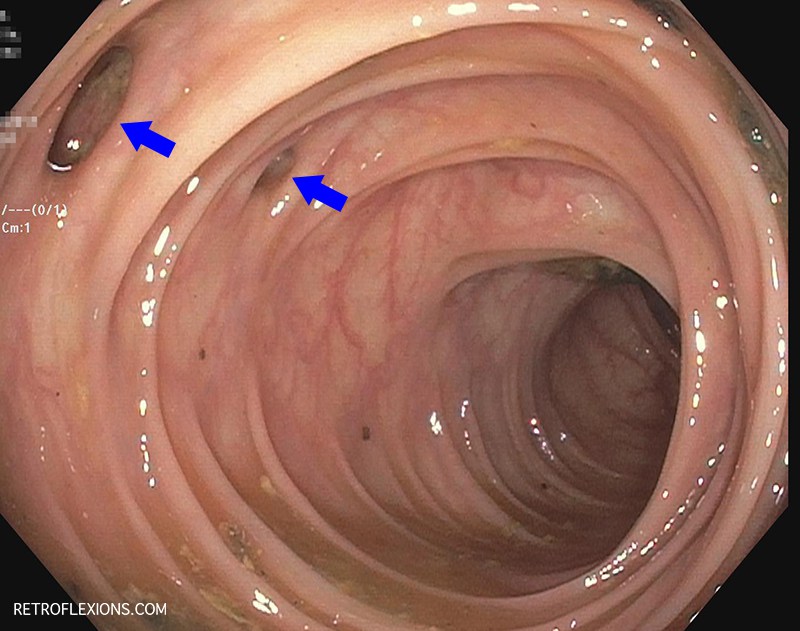
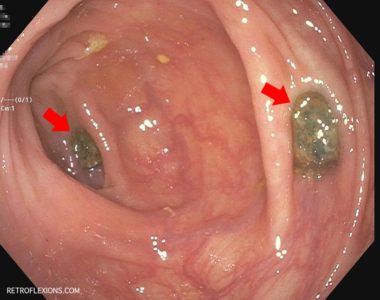
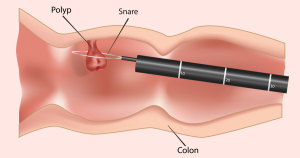
Most people are familiar with colonoscopy, but in case you’re not…colonoscopy is a safe 15-20 minute outpatient procedure that is done using sedation (so it’s painless) that entails using a flexible scope inserted in the rectum (the end part of the colon) and carefully advanced to the cecum (the other end of the colon) to inspect the entire colon lining for the presence of polyps, tumors, and other abnormalities. A polyp is a “precancerous” growth that is common and if not removed can slowly grow and eventually may turn into colon cancer. During a colonoscopy, the doctor can both find polyps and remove these polyps at the same time. Therefore colonoscopy can both diagnose cancer and polyps, but more importantly colonoscopy can prevent colorectal cancer from occurring in the first place by removing precancerous polyps years before they would have otherwise become cancer. A normal colonoscopy typically does not need to be repeated for 10 years. If polyps are found and removed, a colonoscopy will be recommended sooner, to make sure any new polyps that grow will be found and removed before having a chance to turn into colon cancer. Colonoscopy is considered the gold-standard colon cancer prevention test and is the preferred test by most medical societies.
Cologuard® is a non-invasive, commercially-available screening test for colorectal cancer. The test is ordered by a doctor (typically a primary care provider) and mailed to the patient’s house. When the urge to have a bowel movement strikes, the patient places the Cologuard collection device over the toilet and makes a deposit. There are a few simple preparation steps such as adding in a small amount of liquid that the company provides, and then the entire container of poop is mailed back to the company in the provided packaging. The Cologuard test looks for blood and certain DNA mutations in the stool to determine if a test is positive or negative. A week or so later the doctor gets a report indicating the result. If the test is negative, it only “protects” the patient for 3 years.
So which test is better, colonoscopy or Cologuard?
Well, it really depends on what the goals are…
As a general philosophy, it’s much more effective to prevent a disease from occurring rather than waiting for the disease to occur, then reacting to it. When the disease in question is colon cancer, preventing it starts with healthy diet and lifestyle as well as screening the population at large for polyps, the precancerous growths that cause colon cancer. To have a colonoscopy and remove a significant polyp is akin to stopping a future cancer from occurring in the first place. When effective preventive tests like colonoscopy exist, to wait until a patient has developed cancer and then treating the cancer is like waiting until you have been in a car accident to then put on your seatbelt…it’s too late. Although there are excellent treatments available for colorectal cancer nowadays, including surgery and chemotherapy, treating cancer is not the goal of screening. The goal of screening is to not develop cancer of the colon in the first place!
Typically, when an effective prevention technique exists (like removing precancerous polyps during colonoscopy) the earlier we can screen for colon cancer the better. This is why colonoscopy is the preferred test for younger healthier people starting at age 45. Save a 45-50 year old from colon cancer and you will potentially give that person 30-40+ years of life having not developed colon cancer. Saving a 79 year old from colon cancer is still a commendable goal, however the average 79 year old typically won’t have as many quality years left “in the tank” compared to the average 45 year old.
So why does this philosophical stuff matter when it comes to picking a colorectal screening test? Well, understanding what these tests do helps you understand how to apply the proper test to your individual goal.
If this article is already too long and you just want the bottom line, here it is: Colonoscopy is the superior test for most people, especially “younger” people (age 45-mid 70s). It can both detect and (more importantly) prevent colorectal cancer. It is semi-invasive and less convenient when compared to Cologuard testing. Cologuard is an easier test but plagued by false negatives and false positives. Cologuard does not necessarily prevent cancer, it only detects cancer after cancer has occurred, or at best detects large polyps that are close to becoming cancer. Cologuard should be considered for older patients (age 75+), for patients that may not have the best overall health, or for patients who have specific reasons why they cannot have a colonoscopy.
OK, you asked for it! Here are more details, starting with the Cologuard test:
The study that determined the characteristics of the Cologuard test basically performed the test on almost 10,000 patients at average-risk of colon cancer, and then had the patients undergo colonoscopy as the gold-standard test. The results of the Cologuard test were not available to the patients or the endoscopist at the time of the colonoscopy. The major results of this study showed that the Cologuard test had a sensitivity (the amount of times it picked up colorectal cancer when cancer was indeed present) of 92%. It was far less sensitive for picking up advanced precancerous polyps, at only 42%. It turns out that sensitivity is the main thing we care about in a screening test: we want the test to miss none of the patients who have the disease. A perfect screening test would have a sensitivity of 100%, meaning that if 100 people have colon cancer and have the test, all 100 people will get a “positive” test result, meaning no false negative tests.
Sensitivity isn’t everything however…we also want a test that gives a negative result when someone does not have the disease in question. That is, if you take a group of 100 people that do not have colorectal cancer, a perfectly specific test will have 100 “negative” results, meaning no false positive tests.
What does a positive Cologuard test mean?
First and foremost, a positive result on the Cologuard test means that you need to have a colonoscopy. Not a virtual colonoscopy, or another stool test, or another scan of some sort…you need a real optical colonoscopy. Luckily, only about 4% of people with a positive Cologuard test will have cancer found on colonoscopy. 51% will have a precancerous polyp. The rest (45%) will have nothing found on colonoscopy. So to simplify even further, just a little more than half of people with positive results will have something abnormal (cancer or a polyp) found on colonoscopy.
What does a negative Cologuard test mean?
A negative test means that there is a less than one-percent chance of having cancer found on colonoscopy. However, about 34% of people with negative tests still have precancerous polyps found on colonoscopy, with the remainder (66%) of people with negative Cologuard results having truly negative colonoscopies.
What is immediately apparent from these numbers is that Cologuard rarely misses cancer. However, if we count polyps as a significant finding, there are plenty of false-positive results (45%) and plenty of false-negatives too (34%).
A word on how health insurance companies view Cologuard…
While not important to the medical reasoning behind choosing colonoscopy or Cologuard, for some people it is important to note the finances of each test. Either colonoscopy or Cologuard can be considered a screening test, and is typically covered by health insurance plans without an out-of-pocket cost. However, if a Cologuard test is positive (remember that 45% false positive rate discussed above), the insurance company now views the necessary colonoscopy as a diagnostic colonoscopy, not a screening colonoscopy. Diagnostic tests often have an out-of-pocket responsibility for the patient and in the case of a colonoscopy this can be in the thousands of dollars range. This is something rarely discussed when ordering a Cologuard test in the primary care setting, but that we often need to educate patients about when it’s time to book their colonoscopy to follow up a positive Cologuard test.
What about colonoscopy? Are there any downsides?
In good hands, colonoscopy is an excellent test—it’s the best test we have in the fight against colon cancer. However, no test is perfect and colonoscopy is no exception. Even though colonoscopy is the gold-standard test, here are some of the negative things to know about colonoscopy.
Colonoscopy requires a bowel preparation, meaning you have to take either a liquid prep or pill prep to clean out the colon the day before. It’s not painful, but prepping for a colonoscopy is far from a good time. Colonoscopy has small but real risks, such as bleeding, infection, perforation of the bowel, and anesthesia problems. However these risks are very rare, and in with a skilled team the risk of a serious complication is far less than 1 in 1,000 procedures. Colonoscopy also has a miss rate for polyps and even cancer. It is very hard to define an actual number of missed lesions because it’s difficult to perform a study on the gold-standard test (colonoscopy) as there is no better test to compare it to. That being said, colonoscopy can miss small polyps around 20% of the time, and can even miss cancer a few percent of the time. The devil is in the details however: Missing a significant lesion during an outpatient screening colonoscopy in a properly prepped patient (meaning the patient did the bowel cleanse effectively) with a doctor that performs high-quality colonoscopy (meaning the doctor spends adequate time and uses excellent technique to find and remove polyps) is quite a rare event and is something that is difficult to study given variations in quality practice between doctors even in the same community or hospital system.
Here is a quick pros and cons table to help clarify all of the above
| Measure | Colonoscopy | Cologuard® |
|---|---|---|
| Prevention of colon cancer? | Yes | Not really |
| Repeat a normal test every | 10 years | 3 years |
| Overall convenience | Bowel prep and 1 day off work | No prep but have to handle stool |
| Overall invasiveness | Moderately invasive | Not invasive |
| Accuracy | Very accurate | Not very accurate |
| Biggest upside of the test | Better cancer prevention and accuracy | Easy and can do it at home |
| Biggest downside of the test | Bowel prep and less than 0.1% chance of complications | Lots of false positives that will require a colonoscopy anyway |
How do I choose between colonoscopy and Cologuard in my practice?
I typically reserve Cologuard testing for patients that just need to know if they have cancer right now, and are not in good condition to undergo colonoscopy due to other major health issues. A patient that has not been screened recently who is approaching 80 years old, and who has one or more major cardiovascular or pulmonary issues is a good candidate for Cologuard testing. For pretty much everyone else, colonoscopy is by far the better test.
References:
Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med 2014;370:1287-97.
Cologuard website: http://www.cologuardtest.com/current-patients/how-to-use
Cologuard is a registered trademark of Exact Sciences Corporation.